Interactive Activity
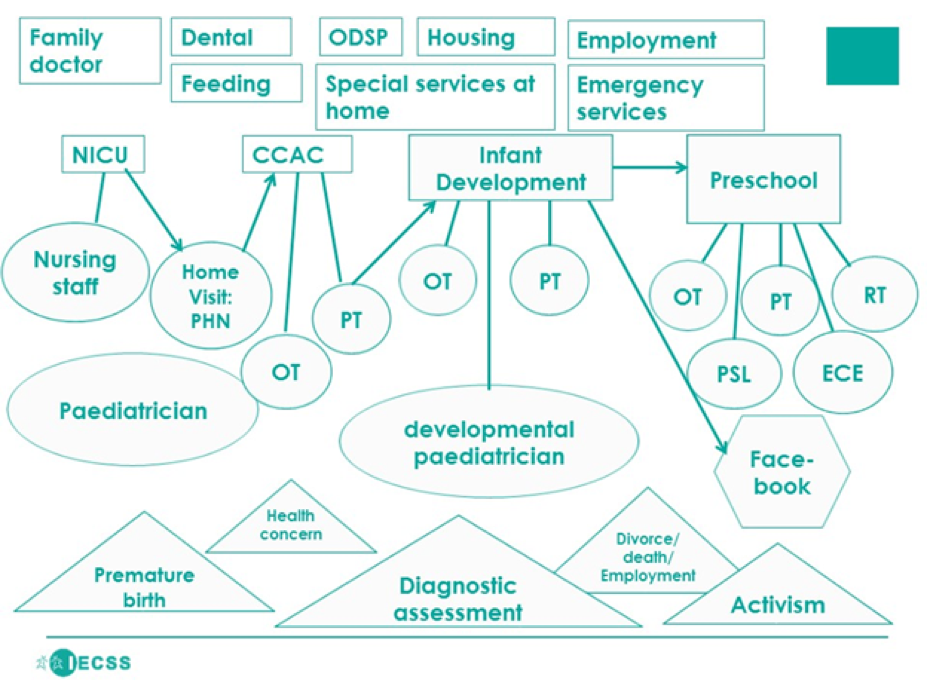
Community maps can be used to show the different services that a family interacts with, highlighting the work that is done by families to navigate multiple services. This community map is not based on a specific family but an aggregated version of what some families experience in several communities (see Underwood, forthcoming for further detail). There are many ways to map family experiences. Some of these include geo-spatial mapping (looking at the geography of services), journey mapping (focusing on the families’ pathway), and eco-mapping (looking at the micro, meso, and macro relationships between the child/student, family and professionals) (Martin, et. al, 2017). The following map was developed using institutional ethnography, a method that seeks to illuminate institutional processes and power through the everyday activities of actors in the system. In this case, the map is drawn from the viewpoint of the family. This approach allows us to see the number of institutions that the family is interacting with, which may be unknown to individual professionals working within single programs or services. The viewpoint of the family, may differ from how the agencies and funders see the services.
Community Map
Below a case study animates the experience of the family represented by this map.
 (Map
first published in Underwood, K., forthcoming)
(Map
first published in Underwood, K., forthcoming)
Map Legend
- OT: Occupational therapy
- PT: Physical therapy
- CCAC: Community Care Access Centre
- ODSP: Ontario Disability Support Program
- PSL: Pre-school speech and language
- ECE: Early Childhood Educator
- PHN: Public Health Nurse
- RT: Resource Teacher
- NICU: Neo-natal intensive care unit
Case Study
The case study animates the experience of the family represented by this map.
Laura was born at 27 weeks gestation. As is usual in this situation, she spent many months in the neo-natal intensive care unit as her lungs developed and medical professionals monitored her development and health concerns. Both of Laura’s mothers interacted with more than 30 health professionals in the hospital before Laura was released to go home. Following their time in the hospital, Laura continued to have regular appointments with a paediatrician, pulmonary specialist, and support for gastro-intestinal development. When Laura was released from the hospital, the family had a home visit from a Public Health Nurse (PHN) within the first 3 days of going home. Through the PHN they connected with Community Care Access Centre (CCAC) in order to get some occupational and physical therapy at home, one day per week. In the first year of being home, Laura was re-admitted to the hospital 3 times, because of ongoing breathing concerns.
The physical therapist who came to Laura’s home became concerned about her development and referred the family to an infant development program. Through this program, a developmental paediatrician diagnosed Laura with Cerebral Palsy. This diagnosis allowed Laura to qualify for more intensive physical and occupational therapy services. Note that the diagnosis was a turning point, from an institutional standpoint. It was required for many of other services that are listed at the top of the map. In the first three years of Laura’s life, her family reports several events that impacted the support they have and their interactions with these institutions. Laura’s grandmother, who had been a regular caregiver and who was very close to Laura, passed away. Laura’s parents separated and then divorced when she was 3 and half years old, and one of her mother’s lost her job with significant financial implications. The family had to stop some private occupational and speech therapy that they had been paying for to supplement the services from the infant development program.
At age 3.75, Laura began attending a pre-school program. Because this program had Occupational Therapy, Physical Therapy and Pre-school Speech and Language supports, Laura no longer qualified for services at the Infant Development program. The preschool also has a Resource Teacher who works with the Early Childhood Educators in the classroom to ensure that the program is adapted for all children/students.
Now, one of the most important supports for both mothers is Facebook page that they learned about through the infant development program. This Facebook page is for parents who have children with disabilities to connect and support each other. Now that Laura is 4 years old, both of her mothers are engaged in activism that is based on the knowledge they have gained from their interactions with these institutions. They support other families by sharing information and helping them to find services.
Note: You can probe whether the diagnosis is in fact necessary or if there are other models that would allow Laura’s family to get the same services with fewer processes, and with recognition of Laura’s development without having a specific diagnosis. Many children/students do not have a diagnosis, or professionals give a vague diagnosis because it will help families to qualify for services. This can lead to inaccurate diagnosis, and an over-reliance on diagnosis as a means of understanding a child’s/student’s “needs” when in fact their development is connected to many factors, including their social, emotional and socio-political surroundings.
Discussion Questions
- Looking at the map, consider how many times a family might: fill out paper work, have to
be “assessed”, have to share personal information, be on a waitlist, or have to develop a relationship
with a professional?
- Note: Each of these “processes” is work for the parent/guardian/or person with responsibility. Each of these processes is also impacted by the social reality of the family. For example, their language, race, socio-economic resources, education, and just “how they present” and their confidence as they interact with institutions.
- Many of these services are only available once there has been a diagnosis, or an assessment of “need”. How does this map then impact the way that disability is constructed in childhood?
- What do you think will happen to Laura when she is old enough to go to school? What transition processes should be in place, and what will services look like in comparison to the early years?
Note: It is important to recognize what is asked of parents, family members and people with responsibility for the child/student. We need to recognize this as work and value it as work, and know that this system only works because mothers, fathers, foster parents, grandparents, and other caregivers are doing work.
Follow-up Questions
- Many of these services are part of a rehabilitation model. Rehabilitation aims to “fix”
impairment. How does the rehabilitation model fit with timely and high quality early childhood
education and care? Are they compatible?
- Note: These services are largely tied to health services, which have different processes than early years services.
- What if a family does not agree with the diagnosis, or the professionals can’t agree on the diagnosis?
- What does this look like if you are not in a “special” preschool? Or, if you live in a geographic area (such as rural or northern communities) where there are not as many agencies?
- What team approach do you think was used between the services in this map? Do you think another approach would have been better?
References
Martin, J., Thompson, A., & Underwood, K. (2016, May). Inclusive Early Childhood Service System Project: Mapping Techniques for Resource Consultants. Poster session presented in the panel Inclusive Early Childhood Service System? at Social Sciences and Humanities Research Congress, Toronto, ON.
Underwood, K. (forthcoming, 2018). A Systems Understanding of inclusive childhoods: The Inclusive Early Childhood Service System project (IECSS). D. Jahr & Robert Kruschel (Eds.) Inclusion in Canada – Perspectives on Cultures, Structures and Practices.